
Consult other specialists as needed (e.g., physical therapist, occupational therapist, nutritionist, social worker).Patients with hip fractures are often admitted to the hospitalist service or internal medicine.Anemia: Consider blood transfusion in symptomatic patients and/or those with hemoglobin 70 years of age are likely best treated in comprehensive geriatrics units (see “ Hip fracture in older adults”).See “ Hip fracture in older adults” for age-related comorbidities. The following conditions are commonly associated with hip fractures and should be managed early as they can impact perioperative outcomes.

Avoid anticholinergics, muscle relaxants, benzodiazepines, and gabapentinoids because they increase the risk of delirium.Ī preoperative peripheral nerve block is recommended to improve pain control and reduce opioid consumption and the risk of perioperative delirium.Use NSAIDs with caution comorbid acute kidney injury ( AKI) is common.Use an opioid-sparing strategy (see “ Acute pain management” for details).Options: femoral block or fascia iliaca block by a trained specialist.Recommended for all patients without contraindications.Perform emergency preoperative assessment.Obtain bedside pelvis x-ray defer other hip imaging until the patient is stabilized.Unstable patients or those with polytrauma.Provide definitive hip fracture treatment based on fracture type (see “Subtypes and variants”).Admit to hospital and begin multidisciplinary care.Manage comorbidities that affect short-term outcomes (see "Acute management of comorbidities”).Obtain hip and pelvis x-rays and other hip fracture diagnostics as needed.Initiate multimodal pain management without delay (e.g., for confirmatory imaging).Identify associated injuries and complications that affect immediate management (e.g., open fracture, fracture-dislocation, neurovascular injury).Early reduction is vital to avoid vascular compromise and sciatic nerve injury. Posterior hip dislocations account for 90% of hip dislocations and typically follow a dashboard injury. Hip fractures can be associated with hip dislocation. Thromboembolism and osteonecrosis of the femoral head are common severe complications. Older adults are at the highest risk of morbidity and mortality early involvement of geriatric care specialists is recommended for these patients. Nonoperative management may be considered for patients with severe comorbidities, although it is associated with a high mortality rate. Management typically includes multidisciplinary consultation, early pain management, IV fluid hydration, venous thromboembolism prophylaxis, and early surgical fixation.

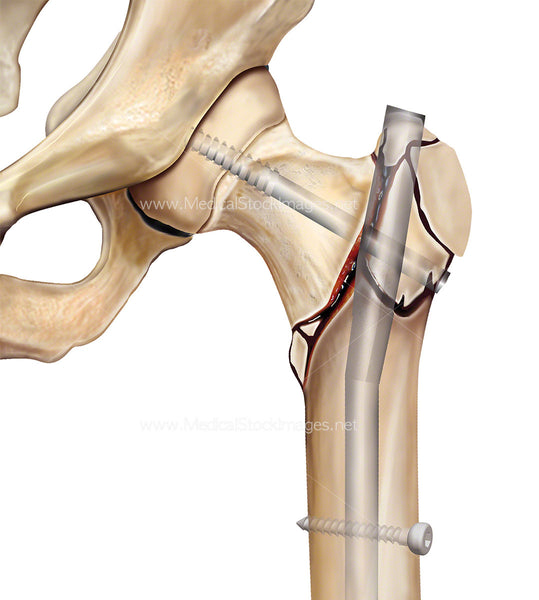
Comorbid conditions (e.g., anemia, acute kidney injury, delirium) are common with hip fractures. X-rays are usually diagnostic, but an MRI may be required to diagnose occult fractures or pathologic fractures. Clinical features include groin pain and deformity of the hip. Hip fractures in younger patients are usually caused by a high-energy impact (e.g., motor vehicle collision). Hip fractures in older adults are typically low-impact injuries and are often associated with osteoporosis. Hip fractures are classified as intracapsular (femoral head, femoral neck) or extracapsular (intertrochanteric, trochanteric, or subtrochanteric).


 0 kommentar(er)
0 kommentar(er)
